Health Care Financing deals with the generation, allocation and use of financial resources in the health system. It is a core function of health systems that can enable progress towards universal health coverage by improving effective service coverage and financial protection. In the current times, for millions of people, these services are not accessible due to the cost. Many others receive poor quality of services even when they pay out of pocket. In the world of gleaming skyscrapers, healthcare services remain a luxury for many.
Particularly in developing nations, due to inadequate infrastructure and limited resources, a large proportion of the population is left vulnerable to preventable diseases and treatable conditions. Even in developed countries, mounting healthcare costs strain individuals’ finances and overburden public systems, pushing essential care out of reach for low-income families and marginalised communities. The consequences turn out to be dire, with delayed diagnoses, untreated illnesses, and increased mortality rates impacting income groups which could least afford it the most.
Framing healthcare as a right or a privilege sparks fierce debate. Proponents of healthcare as a right argue it’s vital for human dignity, societal progress, and even economic efficiency. Denying care based on wealth is unjust, and healthy individuals fuel economies. On the other hand, resources are limited, and some believe personal responsibility and market efficiency should play a role. Ultimately, finding the right balance between individual and societal obligation, affordability, and innovation remains a complex challenge for every society.
Historical Context
Each region has its own unique healthcare history and challenges. But one thing remains constant: “the goal of healthier lives for all” drives the continual evolution of healthcare systems worldwide. Healthcare all over has evolved completely, from ancient roots to the current digitised era.
Early civilizations relied on faith-infused practices, while mediaeval developments like hospitals and Arabic medical scholarship laid the groundwork for scientific revolutions. Vesalius’ anatomical maps, Harvey’s circulation discovery, and Jenner’s revolutionary vaccination forever changed our understanding of the body and disease. The 20th century saw the rise of antibiotics, transplants, and imaging technologies, alongside diverse healthcare systems ranging from socialised models to private insurance. Today, rising costs, antibiotic resistance, and new infectious diseases pose fresh challenges, with access to quality care remaining uneven. Yet, hope lies in cutting-edge technologies like telemedicine, personalised medicine, and AI, offering solutions for a future where everyone has a chance at a healthy life. This ongoing evolution of healthcare continues, driven by the shared aspiration of a healthier world for all.
Along with evolution of the healthcare systems, their working and costs also affected people’s access to healthcare services. Taking the details into consideration, throughout history till present, there are 3 types of financial models which are identified. These 3 models impact accessibility in a different way. The 3 financial models are:
- Government funded model
Under such a model/system, broader coverage is provided at low or no cost at the point of use. Such models promote equity and reduce financial barriers, leading to improved access to everyone, especially vulnerable populations. However, challenges like waiting time and resource crunch can arise.
- Private insurance models
Individuals or employers purchase private insurance plans that cover specific healthcare services. This model can offer choices and flexibility but can also lead to unequal access based on income and employment status due to premium payments. However, in many developing countries, a large portion of healthcare is financed through out-of-pocket payments at the time of service. This can create a major barrier for those with limited financial resources, potentially leading to catastrophic health spending and delayed and foregone care.
- Hybrid model
These are basically combined systems where countries blend elements of public and private financing. It aims to balance equity with individual choice, but the effectiveness depends on the specific design and implementation. These models aim at financial risk sharing and mitigate the burden of catastrophic health expenditure. Such models influence provider networks available to patients, potentially limiting access to specialists or specific types of care.
Overall, healthcare financing models are critical determinants of access to care. Choosing the right model requires careful consideration of the desired outcomes, such as equity, efficiency, and financial protection, to ensure everyone has the chance to live a healthy life.
Healthcare as a right
The case for defining healthcare as a fundamental right is strong. It has to do something with a moral obligation and a dedication to building a just and equal society. The key pillar of this argument is identified as following:
- Dignity and equality: Since health isn’t a privilege, denying someone vital healthcare based on income or social status violates their right to health and well-being. It violates human dignity when you are denied treatment just because you cannot afford it. Universal healthcare recognises the fact that everyone deserves equal access to maintain their health and live a fulfilling life.
- Social Responsibility: When we ensure that every member in the society has access to healthcare, we insure building a healthier and more productive society and this productive society will lead to having a better workforce reinforcing economic growth.
- Economic Efficiency and Long-Term Savings: Unlike the popular opinion, universal healthcare could be economically efficient. Preventive care reduces the need for future treatments, which would be expensive. Also, a centralised public system can negotiate lower drug prices and streamline administrative costs, which therefore leads to saving.
- Breaking the Cycle of Poverty and Vulnerability: Illness can trap individuals and families in a vicious cycle of poverty. Medical debt can detrimentally effect economic security and hinder access to education. Universal healthcare acts as a safety net, preventing illness from pushing people further into hardships.
- A Matter of Justice and Equity: Universal healthcare recognizes that health is a basic human right and not a luxury for the privileged few. By aiming to create a fairer society where everyone could thrive, regardless of their background.
Universally available healthcare
Because universal healthcare is not about a single, static model; it’s about the pursuit of the principle that everyone deserves access to essential healthcare services. Although different countries’ approach may vary, but the goal remains the same which is to build a healthier and more equitable future for all. There are many models available, however choosing the right one depends on a country’s situation and priorities. These systems are:
- Public Healthcare System: It is funded directly by government taxes. This model offers coverage to all citizens regardless of income or employment status. Examples: National Health Service (NHS) in the UK and the single-payer systems in Canada and Scandinavia.
- Social Insurance Model: Like public systems, this model relies on mandatory contributions from employers and employees to a central fund. Germany and Japan are examples, with their multi-payer systems involving private insurance companies.
- National Health Insurance Models: These models lend elements of public and private financing. Where the government acts as a single payer for essential services, while private insurance covers additional benefits or services. Examples: South Korea and Taiwan, offering good access to quality care with some degree of choice.
Healthcare as a privilege
The very idea of healthcare being a privilege, linked to factors like employment, income, or social standing, can feel strange in a world increasingly aware of its fundamental importance. Yet, this perspective persists.
For some, individual responsibility reigns supreme. Maintaining health through good choices and personal diligence is seen as the key to deserving quality care. This perspective often intersects with minimalist philosophies, where minimal government intervention in personal affairs is the preferred path.
Reality, however, paints a nuanced picture. Resource limitations are often “the barrier” to universal access. Prioritising those in immediate critical need or individuals who contribute significantly to the economy (through taxes) becomes a way to manage scarce resources. This perspective, while understandable, raises delicate questions about social justice and the potential for neglecting vulnerable populations.
Historical precedents cannot be ignored. Countries with long-standing private healthcare systems face unique challenges in transitioning towards universal access. Existing infrastructure, established power dynamics, and entrenched financial interests can add layers of complexity to the process, requiring careful consideration and strategic long-term planning.
Navigating the complex landscape of healthcare as a privilege versus a right demands a multifaceted approach. Understanding the ethical and practical nuances of each perspective, acknowledging the role of cultural context and historical legacies, is crucial for informed discussions about the future of healthcare. Ultimately, the pursuit of an equitable system where everyone, regardless of background or circumstance, has access to quality care remains a collective challenge, one that requires ongoing dialogue and innovative solutions.
Bridging the divide
Employing innovative solutions can help in bridging the divide that exists between healthcare being a right or a privilege. The most prominent example of this is Norway, which is generally deemed to have the best healthcare system across the world. Norway’s healthcare system has a dual model – at one level is the social welfare state and the other level involves market based service delivery. The model involves cutting down on bureaucracy, having a universal healthcare system, focusing more on prevention rather than treatment and incorporating technology in healthcare.
On similar lines, India also has healthcare financing working on a dual model of public and private sector. Increasing share of healthcare expenditure as a percent of GDP shows the government’s commitment at making healthcare services affordable and accessible to all. In FY23, the central and state government’s share of expenditure on health rose to 2.1% GDP, which shows progress, but still is lower than other developed nations, like the USA (16.6%), France (12.1%), Germany (12.7%), etc. Moreover, despite the increase in government’s share of expenditure in the Total Health Expenditure (THE), the out-of-pocket expenditure still remains at a high 48.2%, according to the Economic Survey 2023. But the government has launched several schemes and programmes and attempts to lessen the divide in healthcare financing.
Challenges and Barriers
In the course of financing healthcare, there also arise various obstacles. The biggest challenge for India, perhaps, comes due to the lower expenditure on healthcare, compared to the same done by countries around the world. The following figure highlights the difference. Moreover, people are paying more for out-of-pocket expenditure (OOP) compared to what the government is expending for providing healthcare services.
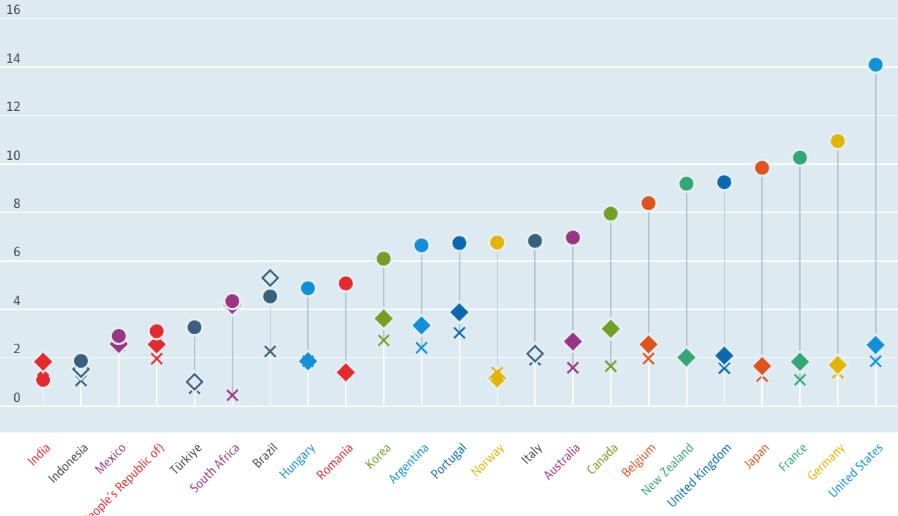
Figure 1: Expenditure on health as a percent of GDP across countries (2022)
Source: OECD (https://data.oecd.org/healthres/health-spending.htm)
Next obstacle can arise from the lack of adequate infrastructure across India. Although the number of primary health centres and community health centres has doubled since the last few years, still some non-metro and remote areas lack the same. The way forward should be to focus on having an adequate number of hospitals, medical professionals, equipment and all other professional equipment accessible to every citizen of the country.
Some barriers can also result from lack of attention being given to healthcare financing by the political class. However, a growing economy, like India, can truly tap into growth and development by giving attention to healthcare financing. As highlighted above, a healthy population is also a growing population economically. Keeping these in mind, since the past few years efforts are being made by the government to increase its expenditure on healthcare.
Lack of awareness regarding the schemes and programmes could also act as a hindrance towards the realisation of healthcare as a right. Hence, this area of efficiently popularising the various government or private health programs also comes into play.
Solutions
The Government of India launched the Ayushman Bharat Programme (2018) aiming towards affordable healthcare and attaining universal health coverage (UHC). One of its components – Health and Wellness Centres, now Ayushman Arogya Mandir (AAM)- aims at providing primary and community healthcare services. The second component – Pradhan Mantri Jan Arogya Yojana (PMJAY) – was to provide 5 lakh cover per family per year of secondary and tertiary treatment to about 500 million beneficiaries. About 90,000 AAMs have been set up in 2022, and till date around 12 crore families avail benefits under PMJAY. Hence, more financing is required to achieve the pre-set targets. However, the efforts are being laid in the correct direction, as the budget allocated for AB-PMJAY in 2023-24 is set to double for FY25.

Figure 2: Components of Ayushman Bharat programme
Source: https://nhm.gov.in/WriteReadData/l892s/84141587321570098109.pdf (UHC brochure)
Healthcare as a right is also realised when people are insured in their dire times, which calls for financing on health insurance schemes. Government insurance schemes (like PMJAY, PMSBY, Central Government Health Scheme) provide cover to the bottom 50% of the Indian population, whereas the upper 20% population can afford the private insurance schemes. But the middle 30% of the population was left uncovered, as they had enough money to pay for nominal premiums but could not afford the private insurance schemes.
Hence, Insurance Regulatory and Development Authority of India (IRDAI), launched Aarogya Sanjeevani insurance product in 2020, which was to be offered by all the insurance companies, sans the deductibles and riders.
However, even today around 30% of Indians do not have insurance, which calls for action from government and private health insurance companies.
Role of Technology
Having innovative solutions to bridge the gap between healthcare financing also means taking into account the role of technology. In India, there are many instances wherein technology is being incorporated in the healthcare sector.
Some prominent examples of this is Electronic Health Records (EHRs), the rising scope of telemedicine services in India like eSanjeevani, Swasth-app (government), or the Tata 1-mg, PharmEasy app by the private sector.
Moreover the role of Artificial Intelligence is also being realised in predicting diseases and helping to subsequently prevent them. The Apollo Hospitals and Microsoft partnered up to design a machine learning model that could give preventive cardiac risk scores.
Technology has the potential of bringing greater convenience for people in healthcare accessing the same. On top of convenience, it would also be affordable, as a report by Accenture highlighted that the Indian healthcare sector might save $4.4 Billion by 2025 due to AI. R S Shamra, CEO of National Health Authority, said that digital transformation in the Indian healthcare system is set to take a more patient-focused approach and make services affordable for them. NITI Aayog is working with Microsoft and Forus Health to design a technology that can detect diabetic retinopathy.
Global Perspectives and Cooperation
There are few examples of some countries that excel in healthcare expenditure, and can set examples for other countries to learn from. For instance, Britain’s healthcare system is the most centrally managed system that is available for the entirety of its population. However, some may argue over the lack of quality being offered or the long waiting times patients need to go through. The Canadian system also finds itself along the same lines – presence of egalitarian services but are costly as well, hence rendering it somewhat deficient.
The Japanese system is different, wherein there is equal contribution from both employer and employee, and it is mandatory for every citizen to have insurance, hence the universal coverage gets ensured. The U.S. healthcare system is known for its quality worldwide, but the issue lies in its affordability and inaccessibility. In China, the delivery as well as the whole healthcare financing mechanism lies with the state, and is found to be efficient. The healthcare financing system of Norway and learnings to be incorporated from it has already been highlighted before.
Hence, each country has different healthcare financing and delivery mechanisms. But from overall experiences, it can be extrapolated that a dual model with government regulated healthcare system along with presence of private players can help to provide the same at reasonable costs while ensuring quality.
India can also learn from these countries, as well as become an example for other countries to follow suit. In fact, the following quote by Prime Minister Modi sums up India’s stance on healthcare financing and importance of global cooperation: “Our goal is to make healthcare accessible and affordable not only to our citizens but for the whole world. Reducing disparity is India’s priority. Serving the unserved is an article of faith for us.”
Conclusion
Healthcare financing is about using finances to be able to provide healthcare services to every citizen. But there also existed the debate between whether healthcare is a right of every person, or remains a mere privilege for the wealthy.
Although both perspectives existed, governments – both at the country and global level- have come to realise the dire need to bridge the gap between right and privilege through targeted healthcare financing. In this process, there arises various obstacles like people still paying majorly out of their pockets to afford health services, or the inefficiency in proper availability of health services.
But every problem follows a solution. Similarly, through rightly targeted expenditure on schemes and programmes, and proper popularisation of the same can act as solutions to bridge the divide.
In this journey of making healthcare more affordable and accessible to people, countries can also learn from each other as highlighted above.
Lastly, a quote that captures the need to bridge the gap between right and privilege, was made by Prime Minister Modi at ‘One Earth One Health – Advantage Healthcare Summit 23’ – “True progress is people centric. No matter how many advances are made in medical sciences, it is vital that access must be assured to the last person at the last mile.”
References:
- Ghebreyesus, T.A. (2017). Health is a fundamental human right. World Health Organization. https://www.who.int/news-room/commentaries/detail/health-is-a-fundamental-human-right
- Gerisch M. (2018). Health Care as a Human Right. American Bar Association. https://www.americanbar.org/groups/crsj/publications/human_rights_magazine_home/the-state-of-healthcare-in-the-united-states/health-care-as-a-human-right/
- heingold, B. H., & Hahn, J. K. (2014). The history of healthcare quality: The first 100 years 1860–1960. International Journal of Africa Nursing Sciences, 1, 18–22. https://www.sciencedirect.com/science/article/pii/S2214139114000043
- Chandrika R. B. (2023). Evolution of the healthcare system in today’s digitalized era. Times of India https://timesofindia.indiatimes.com/blogs/voices/evolution-of-the-healthcare-system-in-todays-digitalized-era/
- Kalmy E. B. (n.d.). Healthcare A Right or Privilege? Mexico Business News. https://mexicobusiness.news/health/news/healthcare-right-or-privilege#:~:text=The%20United%20Sistem%20or%20American,to%20have%20access%20to%20healthcare.
- Kershnar S. (2019). Health care is privilege, not a right. Observer. https://www.observertoday.com/opinion/commentary/2019/03/health-care-is-privilege-not-a-right/
- Suzie (2021). What the NHS can learn from the Norwegian health system. HIN South London. https://hin-southlondon.org/what-the-nhs-can-learn-from-the-norwegian-health-system/
- Ayushman Arogya Mandir (n.d.) https://nhsrcindia.org/sites/default/files/AYUSHMAN%20AROGYA%20MANDIR.pdf
- Health spending. (2017). [Dataset OECD]. https://doi.org/10.1787/8643de7e-en
- Health Insurance for India’s Missing Middle. (2021). NITI Aayog. (https://www.niti.gov.in/sites/default/files/2023-02/Health-Insurance-for-India%E2%80%99s-Missing-Middle_08-12-2021.pdf
- Health Care Financing Practices in Selected Countries. (n.d.). https://www.nipfp.org.in/media/medialibrary/2014/11/HEALTH_CARE_FINANCING_PRACTICES_IN_SELECTED_COUNTRIES.pdf

